Referred Pain: What Is It and How to Treat It
Referred pain is a phenomenon where pain is felt in a location different from its source due to intricate nervous system pathways. Nociceptive signals from the source travel through shared neural circuits, leading to brain misinterpretation. Common causes include nerve impingement, muscle strain, and internal organ issues. Diagnosing referred pain requires thorough clinical evaluation and advanced imaging techniques like MRI and CT scans. Treatment options range from therapeutic exercises and medications to manual therapies and advanced interventions.
Definition of Referred Pain
The human nervous system is intricate and sometimes convoluted. Nerve pathways from different parts of the body often converge at various points within the spinal cord before transmitting signals to the brain. This convergence can lead to the brain's inability to distinguish the precise origin of the pain, resulting in the sensation of pain being 'referred' to a different area. For instance, shoulder pain might actually originate from the diaphragm or heart.
Understanding referred pain is essential for accurate diagnosis and effective treatment. Misinterpreted pain signals can complicate clinical assessments, making it imperative for healthcare professionals to have a thorough grasp of how nerve pathways influence pain perception. This knowledge assists in identifying the true source of pain, ensuring appropriate medical intervention.
Common Causes
Several underlying conditions can lead to the phenomenon of referred pain, each involving complex interactions within the body's nervous system. One of the most important causes is nerve impingement. This occurs when a nerve is compressed by surrounding tissues such as bones, muscles, or tendons. For example, a herniated disc in the spine can impinge on nearby nerves, resulting in pain that radiates to other areas like the legs or arms. Nerve impingement not only distorts normal nerve function but also triggers pain signals that can be felt far from the actual site of compression.
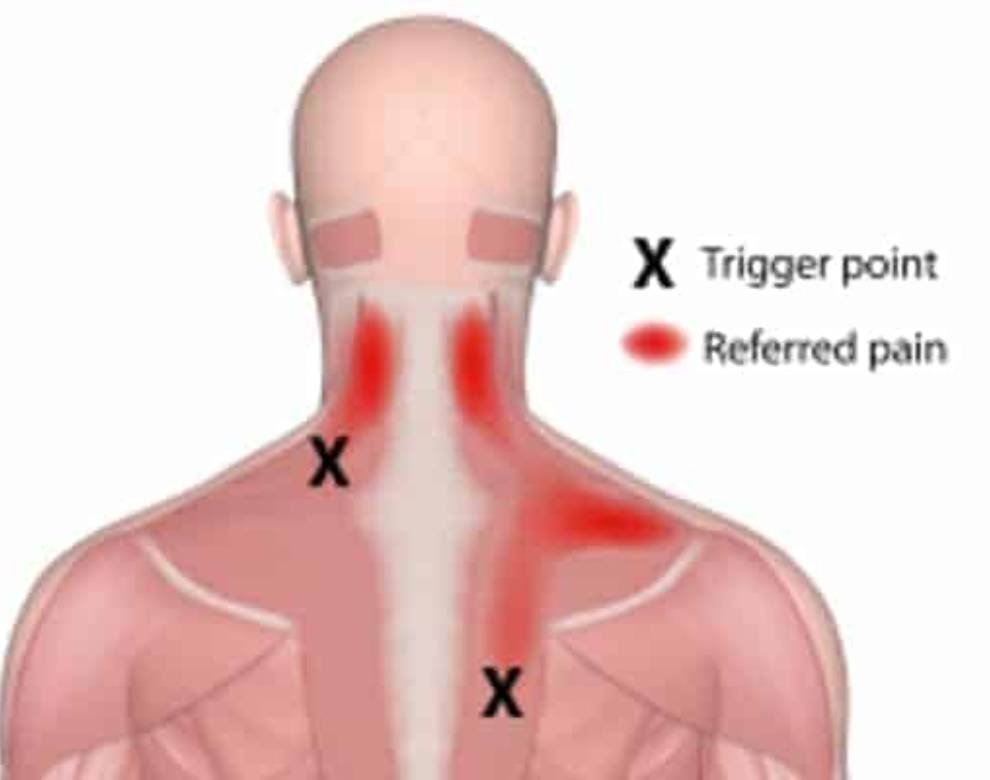
Muscle strain is another common culprit behind referred pain. When muscles are overstressed or injured, they can produce pain that is referred to other parts of the body. For instance, a strain in the upper back muscles could result in pain perceived in the neck or shoulders. This occurs due to shared neural pathways that transmit pain signals from the originally affected muscles to other regions.
Other potential causes include internal organ issues, where pain from organs such as the heart or gallbladder is referred to different body parts. Understanding these common causes is important for effective diagnosis and treatment planning.
Symptoms to Watch For
Identifying the symptoms of referred pain is vital for accurate diagnosis and effective treatment. Referred pain can manifest in areas distant from the actual source of the problem, making it a complex issue to address. Recognizing specific pain patterns is essential for healthcare professionals to pinpoint the origin of discomfort accurately.
For instance, pain originating from the heart may be perceived in the left shoulder or arm, while issues with the gallbladder might cause pain in the right shoulder or scapular region.
Effective symptom tracking involves noting the onset, duration, intensity, and location of the pain. Patients should be encouraged to maintain a detailed pain diary to facilitate this process. Observing whether the pain worsens with certain activities or persists during rest can provide invaluable insights.
Additionally, understanding associated symptoms such as numbness, tingling, or muscle weakness can further aid in distinguishing referred pain from other types of discomfort.
Healthcare providers must be adept at linking these pain patterns and symptoms to potential underlying conditions. By doing so, they can develop targeted treatment plans that address the root cause rather than merely alleviating the referred pain. Accurate symptom tracking is, therefore, a critical step in the effective management of referred pain.
Diagnostic Techniques
Accurate diagnosis of referred pain requires a combination of clinical evaluation, patient history, and advanced imaging techniques. Proper identification begins with a thorough clinical evaluation where the healthcare provider assesses the patient's symptoms, pain characteristics, and physical examination findings. This initial step is essential for differentiating referred pain from other types of pain.
Obtaining a detailed patient history is equally vital. Understanding the onset, duration, and triggers of the pain can provide essential clues. This helps in ruling out other potential causes and directs the focus towards the most likely sources of referred pain.
Advanced imaging techniques and diagnostic tests play a pivotal role in confirming the diagnosis:
• Magnetic Resonance Imaging (MRI): Offers detailed images of soft tissues, aiding in identifying issues such as nerve impingement or muscle injuries.
• Computed Tomography (CT) Scans: Provide thorough cross-sectional images, useful for detecting bone abnormalities or structural anomalies.
• Ultrasound: Utilized for real-time visualization of muscles, tendons, and other soft tissues, helping to pinpoint the origin of referred pain.
Collectively, these methods ensure an accurate diagnosis, facilitating targeted and effective treatment strategies. By integrating clinical assessments with advanced diagnostic tools, healthcare providers can effectively address the complexities of referred pain.
Treatment Options
Effective management of referred pain necessitates a multifaceted approach tailored to the underlying cause and individual patient needs. One cornerstone of treatment is therapeutic exercises, which aim to restore normal function and alleviate pain by targeting the muscles and joints contributing to the referred pain. These exercises often include stretching, strengthening, and range-of-motion activities designed to enhance mobility and reduce discomfort.
Pain management strategies are another critical component. This may involve the use of medications such as nonsteroidal anti-inflammatory drugs (NSAIDs) or muscle relaxants to control inflammation and muscle tension. Additionally, physical therapy modalities like ultrasound, electrical stimulation, and heat/cold therapy can provide symptomatic relief and support tissue healing.
Manual therapies, including massage and chiropractic adjustments, are also commonly employed to address musculoskeletal imbalances and improve alignment. In certain cases, more advanced interventions such as corticosteroid injections or nerve blocks may be necessary to manage severe or persistent pain.
Conclusion
Referred pain is a complex phenomenon where pain is perceived at a location distinct from its source. It can arise from various underlying conditions such as myocardial infarction or spinal nerve compression. Symptoms often include unexplained pain in regions far from the actual pathology.
Diagnostic methods, including imaging and nerve conduction studies, aid in identifying the underlying cause. Treatment approaches range from physical therapy to surgical intervention.
Notably, up to 30% of patients with heart disease experience referred pain, often manifesting in the arm or jaw.
By recognizing the signs and knowing the appropriate treatment options, you can address the root causes and alleviate your discomfort. At Physio Focus, our skilled physiotherapists are dedicated to diagnosing and treating referred pain with personalized care plans tailored to your unique needs. Don’t let referred pain disrupt your life any longer. Book a consultation with Physio Focus today and take the first step towards a pain-free and healthier future. Schedule your appointment now and start your journey to recovery!